| Exam Name: | Certified Documentation Integrity Practitioner | ||
| Exam Code: | CDIP Dumps | ||
| Vendor: | AHIMA | Certification: | Documentation Integrity Practitioner (CDI) |
| Questions: | 140 Q&A's | Shared By: | yasmine |
A resident returns to the long-term care facility following hospital care for pneumonia. The physician's orders and progress note state "Continue IV antibiotics for
pneumonia - 3 more days, after which time the resident is to have a repeat x-ray to determine status of the pneumonia". Is it appropriate to code the pneumonia in this
scenario?
A clinical documentation integrity practitioner (CDIP) is looking for clarity on whether a diagnosis has been "ruled in" or "ruled out". Which type of query is the best option?
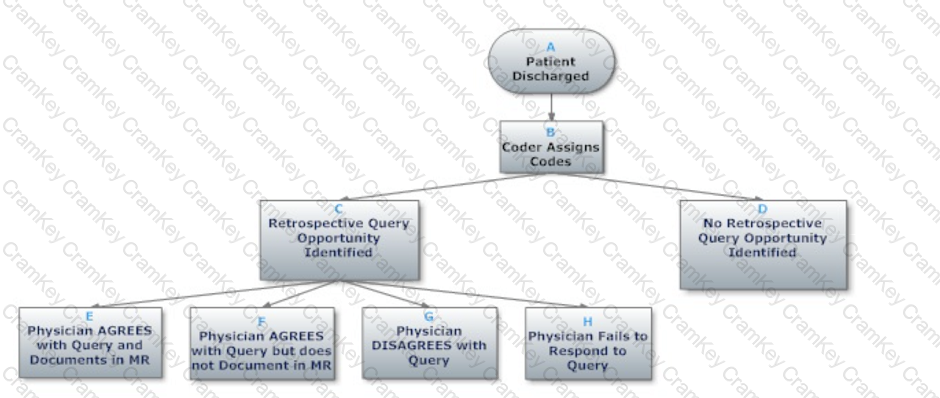
Based on the flowchart below, at what point might the clinical documentation integrity practitioner (CDIP) enlist the help of the physician advisor/champion?